Tachycardia: A Serious Heart Defect
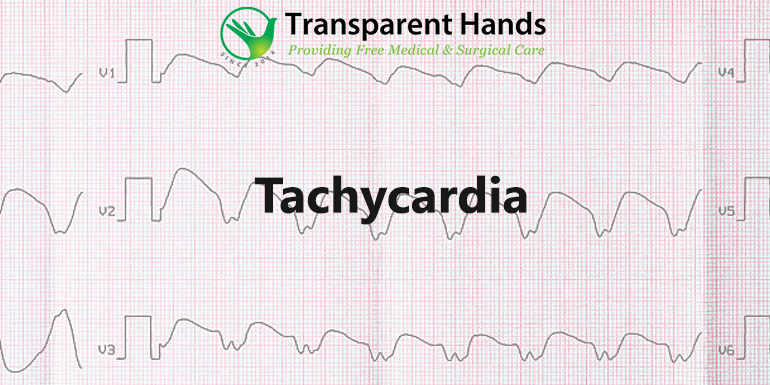
Tachycardia refers to a heart rate of more than one hundred beats per minute. There are several heart rhythm disorders (arrhythmias) that can cause tachycardia.
Sometimes, it is normal for you to have a fast heartbeat. For example, it is common for your heart rate to rise during exercise or in response to stress, injury, or illness. But in tachycardia, conditions unrelated to everyday physical stress cause the heart to beat faster than usual.
In some cases, there may be no symptoms or complications of tachycardia. But if left untreated, tachycardia can interfere with normal heart function and lead to severe complications, including a sudden cardiac arrest or death.
Treatment, such as medication, medical procedures, or surgery, can help control a rapid heartbeat or manage other conditions that contribute to tachycardia.
Types of tachycardia
There are many types of tachycardia. They are classified according to the part of the heart that causes the rapid heart rate and the abnormally fast heartbeat. Common types of tachycardia:
Atrial fibrillation
Atrial fibrillation is a rapid heartbeat caused by chaotic, irregular electrical impulses in the heart’s upper chambers (atria). These signals cause rapid, chaotic, weak contractions of the atrium. It may be temporary, but some episodes do not end if left untreated. This type of fibrillation is the most common type of tachycardia.
Atrial flutter
During atrial flutter, the atrium of the heart beats very fast but at a regular rate. The rapid rate leads to weaker contractions of the atria. An irregular circuit inside the atrium causes atrial flutter.
Atrial flutter episodes may not go away on their own or may require treatment. People with atrial flutter often experience atrial fibrillation as well.
Supraventricular tachycardia
This term refers to an abnormally fast heartbeat that begins somewhere above the heart’s ventricles. It is usually caused by an abnormal circuit in the heart at birth and creates a loop of overlapping signals.
Ventricular tachycardia
Ventricular tachycardia is a rapid heartbeat triggered by abnormal electrical signals in the heart’s lower chambers, i.e., the ventricles. The rapid heartbeat does not permit the ventricles to contract effectively to fill and pump enough blood to the body.
Episodes of ventricular tachycardia may be brief and last only a few seconds without causing damage. But episodes longer than a few seconds can turn into a fatal emergency.
Ventricular fibrillation
Ventricular fibrillation occurs when rapid and irregular electrical impulses cause the ventricles to vibrate instead of pumping the blood needed by the body. If the heart fails to return to normal status within minutes with electric shock (defibrillation), it can be fatal. This type of fibrillation may occur during or after a heart attack. Most people with ventricular fibrillation have underlying heart disease or experience severe injuries such as lightning strikes.
Hyperlipidemia: An Overview
Symptoms
When your heart beats too fast, it may not pump enough blood to the rest of your body. It starves your organs and tissues of oxygen and causes the following signs and symptoms of tachycardia:
- Shortness of breath
- Dizziness
- Rapid pulse rate
- Heart palpitations – rapid racing, uncomfortable or irregular heartbeat or feeling “burying” in the chest
- Chest pain
- Epilepsy
Some people with tachycardia have no symptoms. This condition can only be detected during a physical exam or a heart monitoring test called an electrocardiogram.
When to see a doctor?
Many conditions cause symptoms of a rapid heartbeat and tachycardia. Getting a quick, accurate diagnosis and proper care is very important. If you or your child has any symptoms of tachycardia, consult your doctor.
If you faint, have difficulty breathing, or chest pain lasts more than a few minutes, seek emergency care or dial your local emergency number. Please immediately seek emergency care for anyone experiencing these symptoms.
Tachycardia Causes
Tachycardia is caused by events that interfere with the normal electrical impulses that regulate the pumping action rate of your heart. Many activities or conditions can cause or contribute to a faster heart rate. These include:
- Anemia
- Drinking too many caffeinated beverages
- Drinking too much alcohol
- Do the work
- Fever
- High or low blood pressure
- Electrolyte imbalance, minerals required for conduction of electrical impulses
- Drug side effects
- Hyperthyroidism (hyperthyroidism)
- Smoking
- Sudden stress like fear
- Use of stimulant drugs
In some instances, the exact cause of tachycardia may not be known.
How People with Hearing Disability Can Be Helped?
Risk Factors
- Having a family history of old age, tachycardia, or other heart rhythm disorder makes you more likely to develop tachycardia.
- Conditions that put pressure on the heart or damages the heart tissue can increase your risk of tachycardia. Such conditions include:
- Anemia
- Diabetes
- Heart disease
- Heavy alcohol consumption
- Heavy caffeine use
- High blood pressure
- Hyperthyroidism or dysfunctional thyroid
- Mental stress or anxiety
- Sleep apnea
- Smoking
Complications
Tachycardia problems depend on the type of tachycardia, how fast the heart beats, how long the rapid heart rate lasts, and any other heart conditions that a person might be suffering from. Some of these complications include:
- Blood clots can cause a heart attack.
- Heart failure to pump enough blood
- Frequently fainting
- Sudden death is usually associated only with ventricular fibrillation.
Prevention
The most efficient way to prevent tachycardia is to have a healthy heart and decrease the risk of heart disease. If you already have a cardiac issue, monitor it and follow your treatment plan to prevent tachycardia.
- Exercise and eat a healthy diet.
- Maintain a healthy weight number.
- Keep your blood pressure and cholesterol levels under control.
- If you smoke and cannot quit on your own, talk to your doctor about strategies or programs that can help you quit smoking.
- Drink in moderation
- Do not use recreational drugs. Do not use stimuli drugs. If you need help with ending recreational drug use, talk to your doctor about the appropriate program for you.
- Control stress. Avoid unnecessary stress and learn techniques to deal with regular stress healthily.
- Get regular physical examinations and tell your doctor about any signs or symptoms.
- Monitor and treat existing heart disease
If your symptoms change or get worse symptoms, please inform your doctor immediately.









Leave Your Comments